There is a general presumption, fed by dairy industry advertising, that adequate calcium
is all you need to maintain strong bones. However, several other minerals and vitamins
are also necessary for strong bones, and the absence of any one of them will interfere
with the bone regeneration process. . . . [O]steoporosis prevention and treatment require
a combination of exercise, diet, targeted nutrients, and, in some cases, bioidentical
hormone therapy.
~ Julian Whitaker, MD – 4 Steps to Strong Bones – www.drwhitaker.com
Do you wonder whether you have, or are at risk for, bone disease? Multiple factors determine the extent to which you need to be concerned. An integrative approach that incorporates healthy lifestyle choices, and dietary supplements in the correct doses, may prevent and even reverse bone deterioration.
Causes & Risks for Bone Disease
Uncontrollable Factors. Patients have increased risk for bone disease who are: (1) female (but up to 1 in 4 men age 50+ experience osteoporotic fractures in their lifetimes); (2) menopausal (due to reduced estrogen) or andropausal (due to reduced estrogen and testosterone); (3) Caucasian or Asian; (4) children of parents who had bone disease and/or a hip fracture; (5) small in body frame (due to lower starting BMD); and/or may have (6) excess thyroid hormone (produced or prescribed); or (7) overactive parathyroid or adrenal glands.
Controllable Factors. Risk for bone disease increases in patients who: (1) smoke; (2) drink heavily; (3) are inactive; and/or (4) consumed low amounts of calcium throughout their lives.
Medical Conditions, Procedures, and Treatments associated with a higher bone disease risk include: (1) hormonal imbalances; (2) high blood sugar/diabetes; (3) inflammation; (4) metabolic syndrome; (5) atherosclerosis; (6) gastrointestinal surgery (stomach reduction or intestinal bypass/removal); and (7) long-term or reoccurring intake of various drugs, including corticosteroids (prednisone, cortisone), and those for seizures, acid reflux, and cancer.
Disadvantages of Conventional Drug Treatments
Bisphosphonates (Fosamax, Actonel, Boniva, ReClast) are frequently prescribed to stop bone loss. Since the drugs in this class disrupt the natural bone remodeling cycle (see below), they have demonstrated limited success and are associated with various potential side effects, including: atrial fibrillation; jaw deterioration; thighbone fracture; and digestive ailments (including esophageal ulcers/inflammation).
Conventional practitioners also regularly prescribe synthetic estrogen therapy for post-menopausal women (can increase risk of blood clots, endometrial and breast cancers, and heart disease), or testosterone for andropausal men [can increase risk of stroke, heart attack, and death.
Nutrients Critical to Maintaining Bone Health
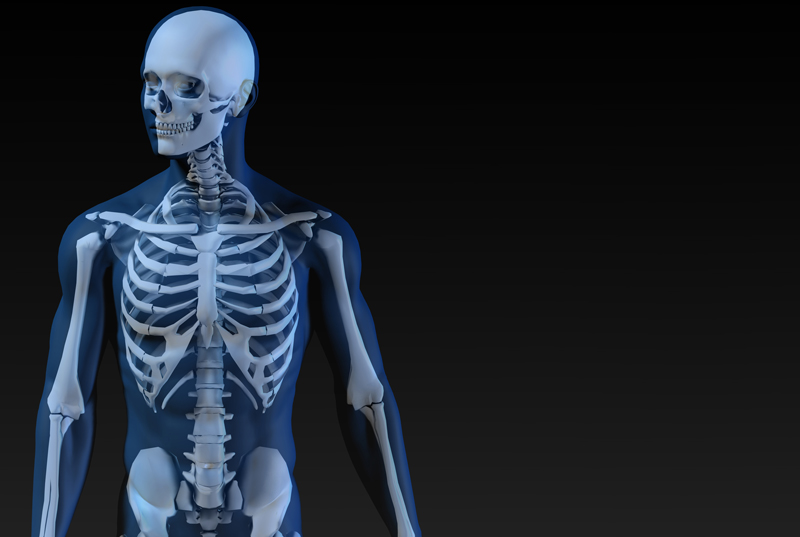
Bone remodeling, a lifelong process that adjusts bone architecture to meet changing mechanical needs and prevent accumulation of old bone, involves three consecutive phases: (1) resorption (osteoclasts digest old mineralized bone); (2) reversal (new cells appear on the bone surface); and (3) formation (osteoblasts lay down new mineralized bone until the resorbed bone is completely replaced).
Robert Heaney, MD, internationally recognized bone biology expert, has especially emphasized the importance of the nutrients discussed below. Numerous comprehensive formulas are available that combine most of the nutrients in a single dietary supplement product. Boosting hormone levels has also proven helpful.
Minerals
Bone is primarily composed of calcium (70%, as hydroxyapatite, a combination of various types of calcium) and matrix protein (30%, see below). According to Heaney, calcium deficiency leads to bone loss, and high calcium intake from food or supplements slows that loss and may even prevent it.
Small amounts of other trace minerals are also essential for normal bone function. These include: magnesium [regulates calcium transport; promotes calcium absorption by converting vitamin D into its active form, 1,25-dihydroxyvitamin D (aka calcitriol)], phosphorous, copper/manganese/zinc, strontium [chemically similar to calcium, and boron.
Vitamin D3
Since vitamin D3 increases the intestinal absorption of calcium, insufficient levels results in depletion of calcium from the bones (and increased deposition of calcium in arterial walls that contributes to atherosclerosis). Experts recommend serum blood levels of 75 nmol/L (or 30 ng/mL), especially to prevent falls and fractures.
Vitamin (K2 & K1)
Vitamin K is available as K1 [phylloquinone; found in green leafy vegetables; absorption is inefficient] and K2 (menatetrenone; includes several menaquinones, including MK-4 in meats, and MK-7 in fermented foods). Vitamin K (especially MK-4 and MK-7) supplementation helps: (1) build the protein matrix that holds calcium in bone; (2) maintain proper bone strength and mineral density; and (3) reduce bone resorption.
Collagen/Silica
Type 1 collagen, a protein molecule that comprises 30% of bone as a spongy matrix of fibers, is critical to achieving optimal bone strength. More collagen in bones means more calcium-binding sites in the bone and greater ability of bone to bend without breaking.
Silica (silicon dioxide) in the form of orthosilicic acid (OSA) is one of the nutrients necessary for optimal production of type 1 collagen, and higher dietary silicon intake is associated with greater BMD in both men and premenopausal women. Research suggests that silicon also regulates bone mineralization by helping to trigger the deposition of calcium and phosphate, reducing osteoclasts, and increasing osteoblasts. A dietary supplement containing choline-stabilized orthosilicic acid (ch-OSA) provides maximum benefits.
Boosting Hormone Levels
Hormones (estrogen, testosterone, and DHEA) monitor bone remodeling. When hormone levels drop in aging adults, bone breakdown in remodeling often exceeds bone building. Julian Whitaker, MD, maintains that supplementing with natural bioidentical hormones can help slow down this process and prevent osteoporosis. Natural estrogen sources include soy isoflavones, black cohosh, and red clover. Natural testosterone boosters include Tongkat ali (Eurycoma longifolia), puncturevine (Tribulus terrestris), and horny goat weed (epimedium).
According to John Lee, MD, international progesterone authority and pioneer, women can increase bone mass and density, and possibly reverse osteoporosis, by using progesterone in the form of a natural transdermal cream derived from wild yams or soybeans. (What Your Doctor May Not Tell You About Menopause 2004)
Some Bone-Supportive Diet & Lifestyle Choices
As noted above, diet and lifestyle choices impact bone health, including: (1) adequate protein intake (per Heaney, above 1.2 g/kg/day, or 25–30 grams/meal, to allow the body to rebuild lost bone and benefit fully from high calcium intake); (2) regular intake of vegetables, fruits, beans, whole grains, and fish; and (3) regular exercise and weight-bearing activities.
The statements in this article have not been evaluated by the Food and Drug Administration (FDA) and are not intended to take the place of a physician’s advice. Unless otherwise supported by specific research and stated herein, the natural remedies discussed herein are not intended to diagnose, treat, cure or prevent any disease.
Submitted by Michael Dworkin, PD, CCN, a Registered Pharmacist and State Certified Clinical Nutritionist (CT Cert. No. 232), with J. Erika Dworkin, Certified Lifestyle Educator and Board Cert. Holistic Nutrition (Cand.). Owner of the Manchester Parkade Health Shoppe (860.646.8178, 378 Middle Turnpike West, Manchester, CT), Pharmacist Dworkin has been guiding patients since 1956 and is available for consultation by appointment. Erika is available to speak to groups. All statements in this article are research-based and references are available upon request.