Many women struggle with estrogen dominance issues and may not even realize it. Symptoms are diverse and include premenstrual syndrome (PMS), mood swings, weight gain, fatigue, breast tenderness, depression with anxiety or agitation, brain fog, headaches, infertility, irregular menstrual periods, irritability, insomnia, polycystic ovaries, sluggish metabolism, water retention and bloating, hypothyroidism, cancer (breast and uterine) and uterine polyps/fibroids. Estrogen dominance does not necessarily mean that one has elevated estrogen levels, but rather insufficient progesterone to balance out the estrogen. Additionally, estrogen dominance may also contribute to endometriosis, blood clots, weight gain, migraines, menstrual cramps, heavy bleeding, and low sex drive.
We are also exposed to xenoestrogens which are considered endocrine-disruptors that have an estrogen-like effect in the body. They come from our environment in products including pesticides, detergents, petroleum products, plastic products and cosmetics. Xenoestrogens may be stored in the fat cells of the body and contribute to estrogen dominance. Some of the more common sources of xenoestrogens are sunscreen lotions; parabens found in many skincare products; bisphenol A (BPA) often found in the lining of cans; phthalates found in plastics; polybrominated biphenyl ethers found in flame retardants; FD&C Red No.3 and the red dye phenosulfothiazine; the food preservative butylated hydroxyanisole (BHA); chlorine; and insecticides. If you are experiencing symptoms of estrogen dominance it might help to switch to organic meats and produce to avoid the various pesticides, reduce the use of plastics (particularly when using a microwave) and switch to organic cleaning and personal care products.
Estrogen and the Menstrual Cycle
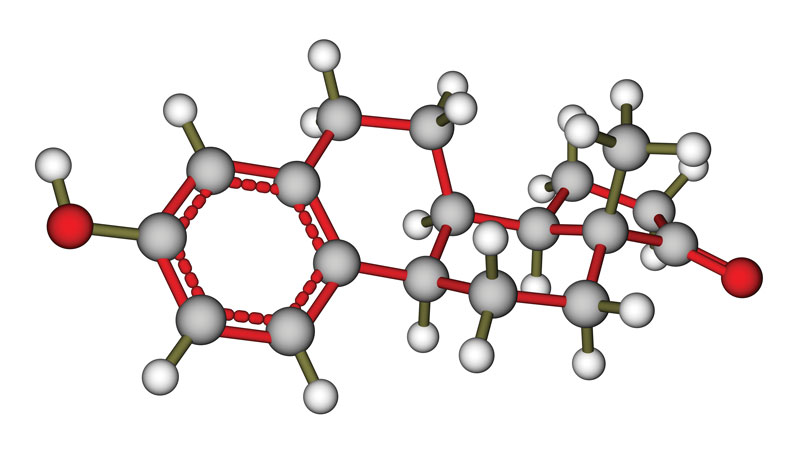
Estrogen is found in many forms in the body. From puberty up until menopause, women move through three phases during their menstrual cycle: follicular phase, ovulation and luteal phase. In the follicular phase, the woman’s menstrual flow begins on cycle day 1 in preparation for ovulation. Here estrogen stimulates the growth of the endometrium so (if fertilization occurs) the blastocyst (newly fertilized egg) may implant. Simultaneously, it allows for the growth and development of a follicle in the ovary that will mature as it leads up to ovulation mid-cycle. The first half of the cycle is also referred to as the proliferative phase and is marked by increasing levels of estrogens and gearing up for ovulation. At ovulation, the egg is released from the ovary into the fallopian tube. At this point, the follicle that it came from becomes the corpus luteum and produces 17β-estradiol and progesterone. This continues either until the placenta is developed in pregnancy or until the uterine lining is once again shed. The corpus luteum hormones serve to stimulate the new uterine lining allowing it to secrete a fluid rich in nutrients in preparation for possible implantation. This half of the cycle is referred to as the secretory phase for this reason. While the follicular phase may vary in length (based on each woman and stress), the luteal phase following ovulation should be exactly two weeks long. If this phase is not two weeks long it is considered a luteal phase defect which is generally caused by insufficient progesterone or when the lining of the uterus does not respond appropriately to the progesterone. If this occurs it may cause more frequent periods, early miscarriage, difficulty getting pregnant and spotting between periods. This defect may be caused by anorexia, endometriosis, too much exercise or elevated prolactin levels (the hormone responsible for milk production). Following ovulation, if a woman is pregnant she remains in the luteal phase until after birth. Otherwise, after two weeks, the cycle repeats and once again she is in the follicular phase.
It is often helpful when experiencing estrogen metabolism issues to chart your cycle to understand your own body’s rhythm and to be able to more effectively communicate your issue with your practitioner. This is actually simple to do. The first day of your period is considered cycle day 1. Mark this on a calendar. Each day, you should take your temperature prior to getting out of bed. During the follicular phase, the temperature should be about a half a degree lower than in the luteal phase (post-ovulation). By doing this you are tracking your basal body temperature and it will be easy to see when and if you ovulate. Conversely, a day prior or the day your period comes the temperature should once again drop approximately half a degree. Other things that you may chart include cervical mucus and position. At the beginning of the follicular phase the mucus is generally thick, white and sticky. As you get closer to ovulation it will begin to thin and become clearer. Right around ovulation the mucus is generally clear and watery or clear and stretchy (like a raw egg white). Following ovulation, the mucus will become thicker again. Similarly, the cervical position changes as the body prepares for ovulation. It is generally low, hard and closed at the beginning of the follicular phase. As you move towards ovulation the cervix will begin to elevate in the vagina and will become softer and more open to allow sperm to enter the uterus. At ovulation the cervix should be high, soft and open. Following ovulation, the cervix position is quite variable. Charting these changes can provide a great deal of information to you and your practitioner. It is also a great way to understand your body, plan for a pregnancy or prevent pregnancy naturally.
Genetically, many of us are predispositioned to having troubles with our estrogen metabolism. We can look to the pathways that break down estrogen to determine risk and/or cause of estrogen dominance.
COMT
Catechol-O-Methyltransferase (COMT) is an enzyme that is most commonly known to breakdown the neurotransmitters (brain chemicals) dopamine, norepinephrine and epinephrine. How is this connected to estrogen, you ask? Well, most enzymes in our body have more than one function. The COMT enzyme is also a part of the estrogen pathway where it helps to breakdown estrogen. This means for those who have a genetic single nucleotide polymorphism (SNP—pronounced “snip”) this will cause decreased function of this enzyme. Since the COMT enzyme is associated with anxiety, women with this SNP find that anxiety increases just before their period. Foods that require activation of the COMT enzyme including coffee, tea, bananas, chocolate, citrus fruits, vanilla, and blueberries may also exacerbate this issue. All enzymes require a cofactor to work effectively. In the case of COMT, this cofactor is the mineral magnesium. Many benefit from supplementing the diet with magnesium in a readily absorbable form such as magnesium glycinate or malate.
PEMT
Phosphatidylethanolamine N-methyltransferase (PEMT) is an enzyme that is use to convert phosphatidylethanolamine to phosphatidylcholine in the liver. Phosphatidylcholine is required for many things in the body including, cell membrane structure, bile secretion and VLDL secretion. In addition to this role, PEMT is also important for the breakdown of estrogen. Since it is also positively affected by estrogen, these mutations generally affect post-menopausal women more strongly than pre-menopausal women. Menopausal women experiencing problems including low or no sex drive, vaginal dryness, and other menopausal symptoms may benefit from phosphatidylcholine supplementation.
Cytochrome P450 Enzymes
The vast amount of our natural detoxification process is done in the liver using the cytochrome P450 system. This is a group of enzymes that actively process toxicants. While we generally think of chemicals, drugs, and other toxicants as substances requiring detoxification, our own hormones, vitamins, and even dietary elements such as protein, cruciferous vegetables and saturated fats require detoxification. These substances require the cytochrome P450 enzymes to help their clearance.
- CYP1A1 is important for the conversion of estradiol to 2-OH-estradiol which is considered the better form of estrogen. Those with SNPs to this enzyme will be less able to convert estrogen to the less toxic form and also generally have higher levels of estrogen.
- CYP1B1 is involved in the hydroxylation of estrogens which helps to prevent hormonally triggered cancers. SNPs can cause an up-regulation of this enzyme causing an increase in the toxic 4-hydroxyestrone intermediary metabolite. If this is combined with COMT SNPs it can really increase the risk of estrogen related cancers and PMS. As this enzyme is also required to metabolize caffeine, I would suggest avoiding caffeine. I would also avoid the substances listed above.
- CYP3A4 is also involved in estrogen metabolism as well as the oxidative deactivation of testosterone.
Since these enzymes are also responsible for detoxifying polycyclic aromatic hydrocarbons (PAH) found in cigarette smoke it is important to stop smoking and to avoid second hand smoke. PAHs are also found in charcoal grilled or broiled meats, so consider wet preparations for meats including poaching and stewing as an alternative. With these SNPs, if you have elevated estrogen it is important to avoid xenoestrogens and endocrine disruptors found in coffee, black tea, chocolate, soy, dairy, flax seed, caffeine, conventional meats and eggs, etc. Supporting the liver with milk thistle and N-actyl-cysteine (NAC) may also be helpful in decreasing estrogen levels. Many women also benefit from the use of diindolylmethane (DIM) supplements as it helps to gently remove excess estrogen by allowing for better detoxification of the hormone. Always ask your doctor or other health practitioner before starting any new supplements. You may learn more about your own genetics by running a genetic test through 23andme. This is a direct-to-consumer saliva test that would allow a qualified practitioner to help you investigate the SNPs mentioned in this article.
Jessica Pizano is the owner of Fit to You, LLC, which offers clinical nutrition and nutrigenomic counseling, as well as personalized training programs. Her concentrations include genetics and nutrigenomics, general health and fitness, weight loss, food allergies/sensitivities, autoimmune disease, mast cell activation disorders, post-rehabilitative work, training/nutrition for medical conditions, obesity intervention, pre- and post-natal exercise and nutrition, and Pilates. She earned a master’s degree in human nutrition that emphasizes functional medicine at the University of Bridgeport. She is a certified nutrition specialist through the Board for Certified Nutrition Specialists. She is continuing her studies at Maryland University of Integrative Health where she is pursuing a doctor of clinical nutrition and is also an adjunct faculty member teaching nutritional genomics. She may be contacted at (860) 321-7234 or online at www.fittoyouct.com.